
Cervical Cancer- Causes, Symptoms, Treatment, Risk Factors, Prevention and HPV Vaccine
Dr. Jahanavi Meena
MBBS, MS ( Obstetrics & Gynaecology)
Senior Consultant, Gynaecology and Obstetrics,
East Delhi Medical Centre
What is the cervix?
Let’s understand cervix itself first. The cervix is the lower part of the uterus, connecting it to the vagina. It serves as a gateway between the uterus and the outside world, playing a vital role in childbirth by dilating to allow the passage of the baby during delivery.
The role is not limited to this. The cervix also produces mucus that helps sperm travel through the reproductive tract to fertilize an egg. Its location and function make it susceptible to various health conditions, including our culprit here- cervical cancer.
Cervical cancer usually begins with the transformation of normal cervical cells into precancerous cells, a process known as dysplasia. Dysplasia refers to the abnormal growth or development of cells within any tissue or organ.
Now a point to note here is that, not all precancerous cells progress to cancer, but while that being said, identifying and treating them early is essential to prevent the development of cervical cancer. This is why screening is important, but more in that later. Over time, if left untreated, these precancerous cells may evolve into cancerous tumors that invade nearby tissues and potentially spread to other parts of the body.
How Does Cervical Cancer Happen?
Cervical cancer typically develops when normal cells in the cervix undergo genetic mutations that cause them to grow uncontrollably.
These mutations can be triggered by persistent infection with certain high-risk strains of the human papillomavirus (HPV), a sexually transmitted infection. HPV can cause changes in the cervical cells, leading to the formation of precancerous lesions. If these precancerous lesions are not detected and treated, they can progress to invasive cancer over time.
Other risk factors for cervical cancer include
- Smoking
- A weakened immune system
- Early sexual activity
- Multiple sexual partners
- A Family history of the disease. Regular screening tests, such as Pap smears and HPV tests, are essential for detecting cervical abnormalities early and preventing the development of cancer.

What are the Symptoms of Cervical cancer?
An important note, Cervical cancer often progresses stealthily, initially devoid of noticeable symptoms, which can complicate early detection. You may not know you have it. However, as the disease advances, certain signs may emerge, indicating its presence. This is why early screening is very important!
Early Stage Symptoms of Cervical
- Postcoital Bleeding: Vaginal bleeding occurring after sexual intercourse.
- Postmenopausal Bleeding: Vaginal bleeding experienced after menopause.
- Irregular Menstrual Bleeding: Bleeding between periods or experiencing unusually heavy or prolonged menstrual cycles.
- Unusual Vaginal Discharge: Watery discharge with a strong odor or containing blood.
- Pelvic Discomfort: Persistent pelvic pain or discomfort, often exacerbated during sexual activity.
Advanced stage symptoms of cervical Cancer
- Rectal Bleeding: Bleeding from the rectum during bowel movements, often accompanied by difficulty or pain during defecation.
- Urinary Symptoms: Difficulty or pain during urination, along with the presence of blood in the urine.
- Back Pain: Dull or persistent backache, unrelated to physical exertion or injury.
- Lower Extremity Swelling: Swelling of the legs, sometimes accompanied by pain or discomfort.
- Abdominal Discomfort: Persistent abdominal pain or cramping, which may worsen over time.
- Chronic Fatigue: Profound and ongoing fatigue, not alleviated by rest or sleep.
However, it’s important to note that these symptoms can also be caused by other, less serious conditions. Regular screenings and prompt medical evaluation are crucial for detecting cervical abnormalities and addressing potential concerns early on.
What are the stages of cervical cancer?
Stage I: At this stage, cancer is localized to the cervix, with no spread to surrounding tissues or organs. The tumor is small and confined within the cervix, making it potentially more manageable with treatment.
Stage II: Cancer has progressed beyond the cervix and uterus but has not yet invaded the pelvic wall or the vagina. Despite this spread, the cancer remains localized to the pelvic region, offering opportunities for targeted intervention.
Stage III: In this stage, cancer has extended to the lower part of the vagina and may have invaded surrounding structures such as the pelvic wall and ureters. Additionally, nearby lymph nodes may be affected, indicating a more advanced disease state that requires comprehensive treatment strategies.
Stage IV: Cancer has metastasized beyond the pelvic region to distant organs such as the bladder, rectum, bones, or lungs. At this advanced stage, the cancer poses significant challenges for treatment and may require a multidisciplinary approach to address both local and distant spread effectively.
Risk Factors for Cervical Cancer
Smoking tobacco: Well I think, everybody is aware of the umpteen number of problems with smoking. We can add this to the list. Smoking significantly increases the risk of cervical cancer, as it can prolong HPV infections (More on that later) and slows the body’s ability to clear the virus. As with all other smoking problems, cease now!
Sexual activity: Engaging in sexual activity at an early age or having multiple sexual partners increases the likelihood of HPV infection, which is the primary cause of cervical cancer. It is imperative that you should prioritize safe sexual practices above all. Additionally, limiting the number of sexual partners will also reduce their risk of exposure to HPV and other sexually transmitted infections (STIs)
Weakened immune system: Individuals with compromised immune systems, due to conditions such as HIV/AIDS or undergoing immunosuppressive therapy, are at greater risk of developing cervical cancer if they acquire HPV. You have to be extra vigilant about preventive measures and undergo regular screenings to detect any abnormalities early.
Exposure to diethylstilbestrol (DES): Those who were exposed to DES in utero, a synthetic hormone prescribed to prevent miscarriage in the past, may have an increased risk of developing clear cell adenocarcinoma, a rare subtype of cervical cancer. Consult with your gynecologist for more information on this. Understanding your medical history and discussing any potential exposure with your doctor for appropriate risk assessment and management is very important.
How prevent Cervical Cancer and Reduce the risk
In terms of prevention, proactive measures can significantly reduce the risk of cervical cancer:
HPV vaccination: The HPV vaccine is a powerful tool in preventing cervical cancer and other HPV-related malignancies. Recommending vaccination to eligible individuals, typically adolescents and young adults, can provide long-term protection against HPV infection and subsequent cervical cancer development. Now, don’t take any internet info or myths related to this! Talk to your doctor.
Regular Pap tests: Routine Pap tests, also known as Pap smears, play a pivotal role in detecting precancerous changes in the cervix early, allowing for timely intervention and prevention of cervical cancer. Emphasizing the importance of regular screenings, starting at age 21 and continuing periodically as recommended, can help identify abnormalities before they progress to cancer.
Safe sexual practices: Encouraging patients to practice safe sex, including consistent condom use and limiting sexual partners, can minimize the risk of HPV transmission and other STIs associated with cervical cancer development.
Smoking cessation: For individuals who smoke, quitting smoking is crucial in reducing the risk of cervical cancer and improving overall health. Healthcare providers can offer support and resources to assist patients in smoking cessation efforts, emphasizing the benefits of a smoke-free lifestyle.
By addressing these risk factors and promoting preventive measures, healthcare providers can play a pivotal role in reducing the incidence of cervical cancer and improving outcomes for their patients.
What is HPV (Human papillomavirus )
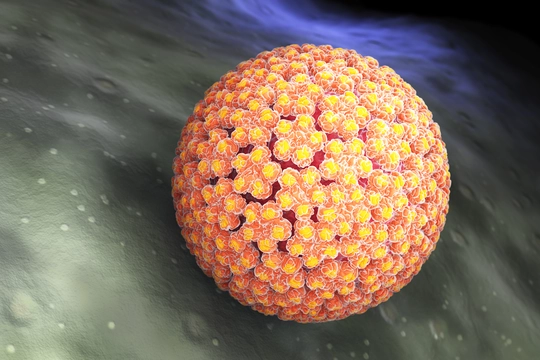
Human papillomavirus (HPV) infection is associated with over 311 000 cervical cancer deaths each year. HPV, or human papillomavirus, is a group of viruses that infect the skin and mucous membranes of humans. It’s one of the most common sexually transmitted infection globally, with 300 million women have an HPV infection in 2016, as cited by WHO. Most HPV infections don’t cause any symptoms and clear up on their own. However, some strains can lead to health issues like genital warts and certain cancers.
You may wonder how HPV affects you. Well, some strains of HPV, known as high-risk types, are particularly concerning because they can cause cancers, including cervical cancer. These high-risk strains are primarily transmitted through sexual contact, whether vaginal, anal, or oral.
Now, here’s the crucial part: persistent infection with high-risk HPV types significantly raises your risk of developing cervical cancer. That’s why understanding HPV and its implications for your health is essential.
But don’t fret just yet! There’s good news. You can take steps to protect yourself. One of the most effective ways to prevent HPV-related health problems, including cervical cancer, is through vaccination. The HPV vaccine is highly effective in preventing infection with the most common high-risk HPV types. It’s typically administered during adolescence or early adulthood, before you become sexually active and potentially exposed to the virus.
HPV Vaccine - What you should know

In the Budget Session, February 2024 Hon’ble Union Minister of Finance Smt. Nirmala Sitharaman announced that the Indian government will encourage HPV vaccination for girls in the age group of 9 to 14 years. Let’s understand this vaccine.
The HPV vaccine, or human papillomavirus vaccine, is a powerful preventive measure designed to protect against infection by certain strains of the human papillomavirus (HPV). The HPV vaccine works by stimulating the body’s immune system to produce antibodies against specific HPV types, providing long-lasting protection against infection..
Types of HPV: The HPV vaccine targets the most prevalent high-risk HPV types, notably HPV types 16 and 18, which are responsible for the majority of cervical cancer cases. These facts are supported by extensive studies and data from reputable health organizations.
How is HPV Vaccine Administered – This is Typically administered in two or three doses, depending on your age and specific vaccine product, the HPV vaccine is most effective when started before potential exposure to HPV through sexual activity.
Recommended age: It’s essential to start thinking about HPV vaccination early. Experts recommend initiating vaccination around age 11 or 12, but it’s never too late to start. Vaccination can begin as early as age 9 and extend up to age 26 for females and age 21 for males who haven’t previously received the vaccine.
Safety: Extensive research and monitoring have consistently shown the HPV vaccine to be safe and well-tolerated. Serious side effects are rare, and any mild reactions, such as temporary pain at the injection site, are normal and expected.
Impact: By getting vaccinated, you’re not only protecting yourself but also contributing to broader public health efforts. Authoritative research demonstrates the significant impact of HPV vaccination in reducing HPV infections and related cancers.
Accessibility: Access to the HPV vaccine is easier than ever. Most health insurance plans cover the cost of vaccination, and many public health programs offer it at low or no cost for eligible individuals. As your advocate, I’ll help you navigate any questions or concerns about affordability and accessibility.
How is Cervical Cancer Treated?
- Surgery: Don’t be scared listening to surgery. It is often the primary treatment for early-stage cervical cancer. The type of surgery recommended depends on the stage and extent of the cancer.
- Conization: Also known as a cone biopsy, this procedure involves removing a cone-shaped piece of tissue from the cervix. It’s often used to diagnose and treat early-stage cervical cancer.
- Simple Hysterectomy: In this procedure, the uterus (and sometimes the cervix) is surgically removed. It may be recommended for early-stage cervical cancer confined to the cervix.
- Radical Hysterectomy: A more extensive surgery that involves removing the uterus, cervix, part of the vagina, and sometimes nearby lymph nodes. It’s typically recommended for larger or more advanced cervical cancers.
Radiation Therapy: Radiation therapy uses high-energy beams to kill cancer cells or shrink tumors. It may be used alone or in combination with surgery for certain stages of cervical cancer. There are two main types of radiation therapy:
- External Beam Radiation: Radiation is delivered from a machine outside the body, targeting the cancerous area.
- Brachytherapy: Also known as internal radiation, this involves placing radioactive materials directly into or near the tumor. It allows for higher doses of radiation to be delivered to the cancer while minimizing damage to surrounding healthy tissue.
Chemotherapy: Chemotherapy involves using drugs to kill cancer cells or stop them from growing. It may be used in combination with radiation therapy (chemoradiation) for certain stages of cervical cancer. Chemotherapy drugs can be administered orally or intravenously.
Targeted Therapy: Targeted therapy drugs work by targeting specific molecules or pathways involved in cancer cell growth and survival. While not yet standard treatment for cervical cancer, targeted therapy may be used in clinical trials or in cases where standard treatments have been ineffective.
Immunotherapy: Immunotherapy uses the body’s immune system to fight cancer. It may be used in clinical trials or as part of personalized treatment approaches for advanced cervical cancer.
Who treats Cervical Cancer?
Navigating cervical cancer treatment involves a dedicated team of specialists, each bringing their unique expertise to your care journey:
- Your Gynecologist: Your gynecologist, someone you likely already trust with your reproductive health, will be a constant presence throughout your treatment. They’ll guide you through the diagnosis process and ensure you understand your options every step of the way.
- Your Gynecologic Oncologist: This specialist focuses solely on cancers of the female reproductive system, including cervical cancer. With their advanced training and experience, they’ll provide personalized treatment recommendations and coordinate your care seamlessly.
- Your Radiation Oncologist: Working behind the scenes, your radiation oncologist will craft a tailored radiation therapy plan to target the cancer while minimizing impact on healthy tissues. Their expertise ensures that each treatment session is as effective and comfortable as possible.
- Your Medical Oncologist: Your medical oncologist will be there to explore additional treatment options, such as chemotherapy, and provide ongoing support as you navigate the challenges of cancer treatment. They’ll collaborate closely with your other doctors to ensure a holistic approach to your care.
But remember, you not need everyone here or in many cases, you may need only one doctor. Each case is different.
Can cervical Cancer Kill?
WHO states “When diagnosed, cervical cancer is one of the most successfully treatable forms of cancer, as long as it is detected early and managed effectively. Cancers diagnosed in late stages can also be controlled with appropriate treatment and palliative care.”
We don’t have to lose hope the moment we or our loved gets this diagnosis. With timely diagnosis, appropriate treatment, and ongoing medical care, the prognosis for cervical cancer has improved significantly, offering hope and the possibility of a positive outcome for many patients. It’s important for individuals to discuss treatment options and expectations with their healthcare team to develop a personalized treatment plan tailored to their specific needs and circumstances.
Sources
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018 Nov;68(6):394-424. Epub 2018 Sep 12. Erratum in: CA Cancer J Clin. 2020 Jul;70(4):313.
https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
https://www.cancer.gov/types/cervical
