Glaucoma- the Why, What and How of the "Silent Thief of Sight"
Dr. Ashwini Jain
MBBS, MS, OPTHALMOLOGY
DOMS – Senior Consultant, Ophthalmology – EDMC
What is the Glaucoma?
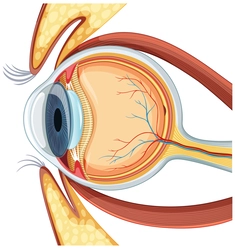
Glaucoma is group of Eye Diseases/Disorders that affect the Optic Nerve of eyes and may lead to vision loss if left unchecked. The definition itself may sound ominous, but I would like to remind you of the condition – If left unchecked. Let’s Start with Optic Nerve
What is optic nerve and what is Optic Nerve Damage?
Origin Story – Cranial Nerves
Optic nerves are a part of Cranial Nerves which are a part of Central nervous system!
Cranial nerves emerge directly from the brain, facilitating sensory perception, motor control, and autonomic functions. You are able to see, hear, sense touch due to these nerves. There are total 12 pairs of Cranial nerves. Each pair has branch to left brain and other to right brain. Among the twelve pairs of cranial nerves, the optic nerve, designated as Cranial Nerve II, holds a unique position as the primary medium for visual information transmission. The optic nerve originates from the retina, the light-sensitive layer of tissue lining the back of the eye.
What do Optic Nerves Do?
The primary function of the optic nerve is transmitting visual information from the retina to our brain for interpretation. Light signals captured by the retina are converted into electrical impulses that travel along the optic nerve fibers. The red you see is perceived and identified as red because of Optic nerve!
Additionally, you must have heard or read about how the pupil dilates as a response to change in light conditions and other factors, this is also facilitated by optic nerves.
How Does Glaucoma affect Optic Nerves?
In the Eye there is a continuous production and drainage of a transparent fluid known as aqueous humor. This fluid is important to eyes as it circulates within the anterior chamber, nourishing the surrounding tissues before exiting through specialized channels located in the cornea and iris.
Although, when these drainage pathways encounter obstruction or blockage, the natural pressure within the eye, called intraocular pressure (IOP), can elevate. As the IOP rises, it exerts undue pressure on the optic nerve, resulting in gradual damage over time. This progressive nerve damage compromises visual function, leading to the onset of vision loss and potential blindness in the affected eye.
Before going back to optical nerves, let’s see the types of Glaucoma

What are the Symptoms of Glaucoma?
National Eye Institute in its 2014 Press Release termed the disease “Silent thief of Sight” – Because more often than not, this disease does not have any symptoms in the beginning and you may go years without feeling anything while the diseases slowly progresses. This is not to scare you, but to simply stress on the importance of regular visits to your Ophthalmologist.
Here’s a breakdown of the symptoms associated with different types and stages of this sight-stealing condition:
Open-Angle Glaucoma:
- Initially asymptomatic
- Gradual onset of patchy blind spots in peripheral vision
- Advancement to difficulties in central vision perception in later stages
Acute Angle-Closure Glaucoma:
- Severe headache
- Intense eye pain
- Nausea or vomiting
- Blurred vision
- Perception of halos or colored rings around lights
- Eye redness
Normal-Tension Glaucoma:
- Early stages may be symptom-free
- Gradual progression to blurred vision
- Later stages may entail loss of peripheral vision
Glaucoma in Children:
- Infants may present with a dull or cloudy eye
- Increased blinking or tears without crying
- Blurred vision
- Worsening nearsightedness
- Headaches
Pigmentary Glaucoma:
- Perception of halos around lights
- Blurred vision exacerbated by physical exertion
- Gradual loss of peripheral vision
Please note, the symptoms of glaucoma vary depending on the type and stage of the condition. While some forms may progress silently, others manifest with pronounced symptoms necessitating immediate medical attention. You cannot self-diagnose, this article is for information only and not for you to diagnose or be relaxed without a proper checkup. Regular eye examinations serve as a crucial tool in detecting glaucoma early, thereby preserving vision and stopping any of its potentially devastating consequences.
What are the Types of Glaucoma?
Open-angle glaucoma is the most prevalent form, affecting a vast majority of individuals diagnosed with glaucoma worldwide. This condition develops gradually, characterized by a buildup of resistance within the eye’s drainage canals. Despite appearing open and functional, these canals gradually accumulate fluid, elevating intraocular pressure (IOP) and exerting stress on the optic nerve. Often asymptomatic, open-angle glaucoma can remain undetected for extended periods.
Closed-angle glaucoma, also known as angle-closure or narrow-angle glaucoma, manifests abruptly and infrequently. This is a rare variant which occurs when the angle between the iris and cornea narrows, typically triggered by rapid pupil dilation. The constricted angle impedes proper drainage, leading to a swift rise in intraocular pressure. Symptoms of closed-angle glaucoma, such as eye pain and headaches, necessitate urgent medical attention due to their severity.
Normal-tension glaucoma poses a unique challenge, as optic nerve damage occurs despite normal or moderately elevated eye pressure. This puzzling condition, also referred to as normal-pressure or low-tension glaucoma, perplexes experts regarding its underlying causes. It appears to be more prevalent among individuals of Asian descent.
Lastly, congenital glaucoma manifests in infants born with improperly formed drainage canals, a condition often detected shortly after birth or during early childhood. Also known as childhood, infantile, or pediatric glaucoma, this variant requires prompt medical intervention to prevent irreversible vision impairment.
Who is at Risk for Glaucoma?
Age: Studies have shown that individuals over the age of 60 are at higher risk for developing glaucoma, with the prevalence of the disease increasing with advancing age. (1) The aging process brings about physiological changes in the eye, including alterations in aqueous humor dynamics and decreased resistance to optic nerve damage, rendering older adults more vulnerable to glaucomatous pathology.
Genetic Predisposition: The genetic underpinnings of glaucoma have garnered increasing attention in recent years. Family history of glaucoma emerges as a potent predictor of disease risk, with individuals having relatives diagnosed with glaucoma at heightened susceptibility. Genetic studies have identified several gene variants associated with glaucoma susceptibility. (2)
Race and Ethnicity: Glaucoma exhibits marked racial and ethnic disparities, with certain populations bearing a disproportionately higher burden of the disease. Studies have revealed a significantly higher prevalence of glaucoma among individuals of African, Hispanic, and Asian descent compared to Caucasians.
Medical Conditions and Medications: Certain medical conditions and medications pose additional risk factors for glaucoma development. Chronic conditions such as diabetes and hypertension have been linked to an increased risk of glaucoma, likely due to their systemic effects on ocular perfusion and vascular health. (3) Prolonged corticosteroid use, whether topical, oral, or inhaled, has also been associated with elevated intraocular pressure and an increased risk of glaucoma development. (4)
Conclusion: As healthcare providers, it is our duty to identify and mitigate the risk factors contributing to glaucoma development. By recognizing the individuals most vulnerable to its grasp—whether by age, genetics, race, or medical history—we can implement targeted screening and intervention strategies to preserve vision and improve patient outcomes. Through ongoing research, education, and advocacy, we strive to unravel the complexities of glaucoma and safeguard the sight of generations to come.
How is Glaucoma Diagnosed?
Let’s understand the tests your doctor may suggest you if you visit them for an eye check p. These tests are often done by your doctor when she or he may suspect something is wrong because the pressure of the eye may seem off or due to your medical history.
- Dilated Eye Examination:
- This procedure involves the administration of eye drops to dilate the pupils, enabling a thorough examination of the optic nerve at the back of the eyes.
- Sources: American Academy of Ophthalmology, Glaucoma Research Foundation
- Gonioscopy:
- Gonioscopy is employed to examine the drainage angle where the iris and cornea meet, providing insights into the mechanism of intraocular fluid drainage.
- Sources: Glaucoma Research Foundation, National Eye Institute
- Optical Coherence Tomography (OCT):
- Utilizing advanced imaging technology, OCT enables the visualization of structural changes in the optic nerve, aiding in the early detection of glaucoma.
- Sources: Investigative Ophthalmology & Visual Science, Journal of Glaucoma
- Ocular Pressure Test (Tonometry):
- Tonometry measures intraocular pressure (IOP), a critical risk factor for glaucoma, by assessing the pressure within the eye.
- Sources: American Academy of Ophthalmology, Glaucoma Research Foundation
- Pachymetry:
- Pachymetry involves the measurement of corneal thickness, as corneal thickness can influence intraocular pressure measurements and glaucoma risk assessment.
- Sources: Journal of Glaucoma, American Optometric Association
- Slit-Lamp Examination:
- This examination utilizes a specialized microscope called a slit lamp to examine the internal structures of the eye, providing detailed insights into ocular health.
- Sources: British Journal of Ophthalmology, American Academy of Ophthalmology
- Visual Acuity Test (Eye Charts):
- Visual acuity tests, commonly performed using eye charts, assess an individual’s ability to discern letters or symbols at various distances, aiding in the evaluation of vision loss.
- Sources: American Optometric Association, Mayo Clinic
- Visual Field Test (Perimetry):
- Performed through visual field testing, or perimetry, evaluates changes in peripheral vision, crucial for detecting early signs of glaucoma-related vision loss.
These tests may be done in combination, so we can effectively assess glaucoma risk. If you are reading this, there is a good chance you may have already gone through some of these tests. You have nothing to worry, these tests would be repeated every few months if you have glaucoma or a medical history. They will make sure this silent thief is not silent anymore.
How is Glaucoma Treated?
Let me start with something ominous, something you have heard from your doctor already, Glaucoma is not reversible.
While it remains an incurable condition, its progression can be effectively managed through a combination of therapeutic modalities tailored to individual patient needs.
Many individuals take eye drops and maintain their eye health for the rest of their lives. By diligently adhering to prescribed treatment regimens and undergoing regular follow-up evaluations, individuals afflicted with glaucoma can optimize their visual sense and live a normal life.
What is best for you, will be determined by your doctor, but let’s get to know the different conditions! And for those of you who are throwing scared glances at the surgery section, Most of the cases only need Eye drops!
- Prescription Eye Drops:
- Prescription eye drops constitute the cornerstone of glaucoma management, with diverse formulations targeting different aspects of intraocular pressure regulation.
- Some eye drops enhance aqueous humor outflow, while others reduce its production, collectively contributing to IOP reduction.
- Sources: American Academy of Ophthalmology, Glaucoma Research Foundation
- Oral Medications:
- In cases where eye drops alone prove insufficient in achieving target IOP levels, oral medications may be prescribed as adjunctive therapy.
- Carbonic anhydrase inhibitors are commonly utilized oral medications, albeit with potential side effects including gastrointestinal disturbances and renal complications.
- Sources: Mayo Clinic, National Eye Institute
- Laser Treatment:
- Laser therapy offers a minimally invasive alternative for lowering intraocular pressure, often employed as a primary or adjunctive treatment modality.
- Procedures such as selective laser trabeculoplasty (SLT) and laser peripheral iridotomy (LPI) facilitate improved aqueous humor outflow, thereby reducing IOP.
- Sources: British Journal of Ophthalmology, Journal of Glaucoma
- Surgical Intervention:
- Surgery may be warranted in cases where medical and laser therapies fail to adequately control intraocular pressure or in advanced stages of glaucoma.
- Traditional surgical procedures, including trabeculectomy and tube shunt implantation, aim to enhance aqueous outflow by creating alternative drainage pathways.
- Minimally invasive glaucoma surgery (MIGS) represents a burgeoning field, offering less invasive approaches with reduced postoperative complications and faster recovery times.
Conclusion
By staying proactive with regular eye check-ups and adhering to prescribed treatment plans, individuals diagnosed with glaucoma can significantly slow the progression of the disease and maintain their vision. You don’t have to panic. With proper care and support, individuals living with glaucoma can confidently face the future with optimism, knowing that they have the resources and expertise needed to preserve their vision for years to come.
Sources
- National Eye Institute. (2020). Glaucoma: Who is at risk for glaucoma? Retrieved from https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/glaucoma/who-risk-glaucoma
- Wiggs, J. L., & Pasquale, L. R. (2017). Genetics of glaucoma. Human Molecular Genetics, 26(R1), R21–R27.
- Tham, Y. C., Li, X., Wong, T. Y., Quigley, H. A., Aung, T., & Cheng, C. Y. (2014). Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology, 121(11), 2081–2090.
- Rhee, D. J., & Ramos-Esteban, J. C. (2006). N. Engl. J. Med. 354, 17: 1803-1805.
<a href=”https://www.freepik.com/free-vector/diagram-human-eyeball-anatomy_13832801.htm#fromView=search&page=1&position=0&uuid=6e07eaaf-61b3-41e0-957a-7b911415c64c”>Image by brgfx on Freepik</a>
